How 21st technology can enable patient-centric enrollment process
Patients are 21st century consumers. Here's what they expect.
Being patient-centric in clinical trial operations is much more than just a trend and a buzzword. In a world where consumers can instantly book a ride, order groceries, and find their next vacation stay from their phones, patients expect similar experiences - seamless, user-friendly, fast - in their healthcare.
The clinical trial enrollment process needs to step up to meet the expectations of interested patients. And by learning from the aforementioned services, clinical trial sponsors and sites can uncover valuable lessons in how to leverage modern technology to better recruit and retain study participants.
The need for a new approach
Delays in patient recruitment are one of the main barriers that prevent medical breakthroughs from reaching patients. More than 85% of clinical trials failing to complete enrollment within their forcasted timeframe, and according to the FDA, only 6% of clinical trials meet enrollment timelines.
For treatments where each day of delay costs can sponsors on millions in forgone future sales, the need to optimize recruitment is clear.
At Clara, we've worked directly with thousands of patients in the course of building our software. It's become clear to our team through the course of this work that designing for the modern patient and addressing their needs as an Airbnb or Uber would address the needs of their billions of users is a tactic that can help fix many of the shortcomings of our industry's current processes.
The 21st century patient in a 20th century industry
With over 43% of people today using the internet as their go-to source for health and wellness information, and 1 in 20 Google searches being related to health, the digital age has created a fundamental paradigm shift in trial recruitment. Medical information is increasingly accessible online; as a result, the CISCRP finds that patients today are more and more likely to learn about clinical trials from Doctor Google and reach out to sites on their own, without the guidance they have when the trial is being introduced by a physician.
While this can allow sponsors and clinical trial sites to expand their reach beyond patients already being seen at the study sites, the traditional enrollment process hasn’t adapted to this change. Patients face numerous barriers, and in the end, many qualified candidates drop-off before enrolling in the trial out of frustration.
The consideration of the patient journey in trial recruitment can make a sizeable impact on whether or not a patient enrolls in a trial -- designing without empathy or insight into a typical patient’s journey will cause your recruitment funnel to spring unnecessary leaks. It is paramount to remember that these patients have full lives, outside of their medical conditions: Families, jobs, and, yes, a desire to go to happy hour with some friends. It is unreasonable to force them through a gauntlet of unreturned phone calls and emails that are answered only a week after the fact.
Both sides of the table
Because we build software and resources for both the patient and the researcher, our team works with every party in the ecosystem: Patients, trial sites, and sponsors.
By working with all manner of patients, from the super engaged advocate to the frustrated senior citizen on Medicaid, and walking in their shoes, we learned firsthand what makes a given trial’s enrollment process straightforward and engaging...and what makes one frustrating or downright impossible to navigate. And by working closely with coordinators at independent trial sites, researchers at major research hospitals, and executives at major pharmaceutical companies, we learned about the hurdles that exist for everyone on the research side of the equation: What these hurdles are, why they exist, and how they are currently navigated by teams that are often stretched thin.
All this to say this: We've listened to everyone involved, and it is our belief that patient-centricity can be something near a panacea for everyone in this space. And luckily, the 21st century has brought about a wealth of tools that anyone can use to build patient-friendly enrollment flows that help decrease the workload for teams and accelerate trial recruitment.
How it is
The 20th century funnel
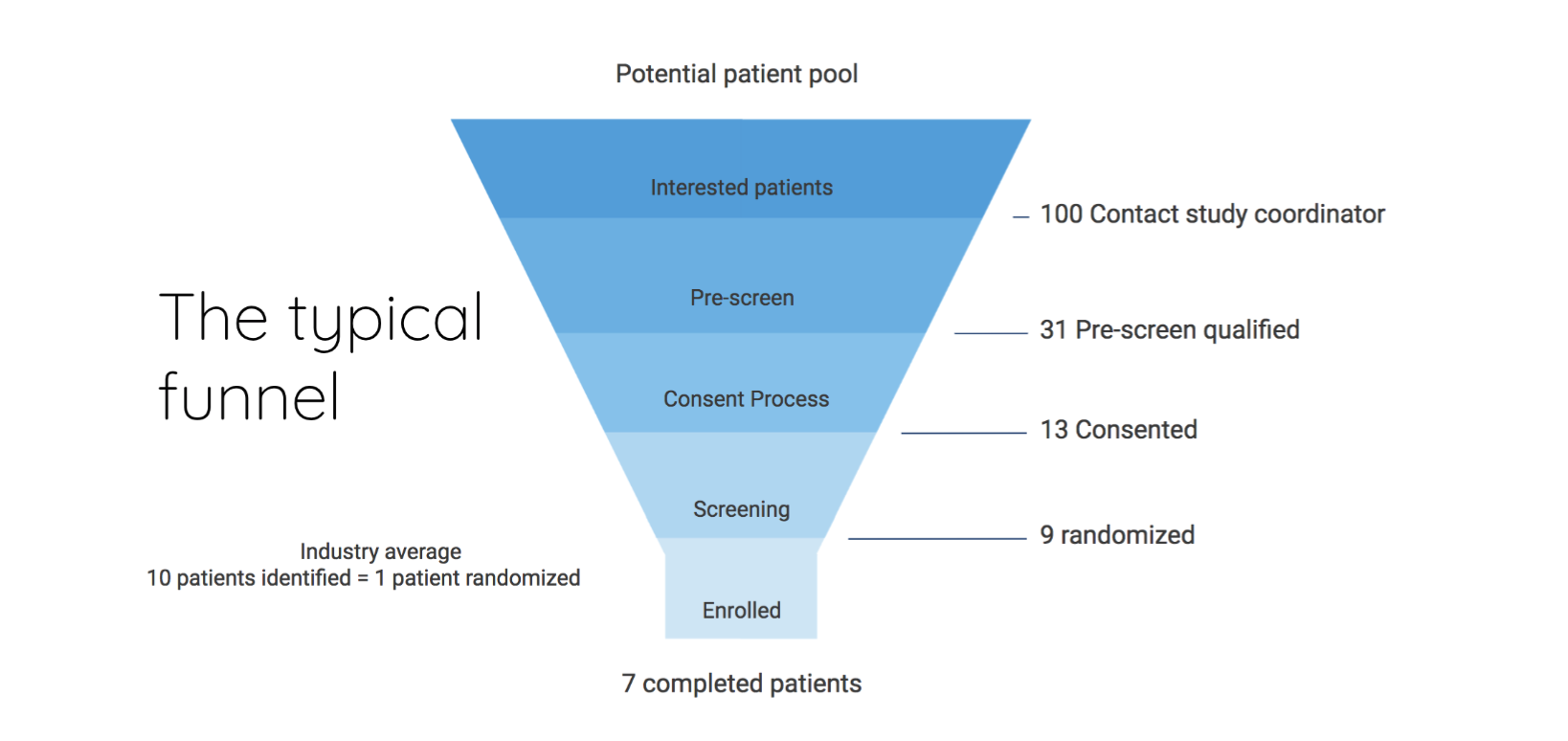
This should look familiar. It's the average recruitment funnel, starting with candidates who may be interested in your clinical trial, and gradually working down to the very few who make it all the way to enrollment.
There are two main ways to get more patients all the way through to enrollment:
-
Spend more money and effort to increase the number of patients in the top of the funnel.
-
Maximize the impact of the dollars and person-hours spent by plugging the holes.
In truth, every recruitment effort needs to look closely at both solutions and arrive at a mix of the two. In this guide, we'll spend time on working through how to improve the latter through a mix of technology and patient-centered design.
Some of this drop-off is unavoidable due to patients at the top of the funnel not fitting the eligibility criteria. However, a surprising and significant amount of drop-off occurs from eligible candidates falling through the cracks because the trial’s enrollment solution does not address their needs at each step of the funnel.
Granted, there are time and resource constraints - not to mention restrictions placed by the sponsor, site management, the IRB, etc. - that make it difficult to implement the recruitment experience everyone ideally wants to be delivering to patients. It is much more difficult to implement new processes once a trial is in the middle of its run; we recommend using these principles from the very start, as your team scopes out and designs the way your trial will recruit and operate.
Let's now dive into the difficulties patients face, and break down a series of fixes that can be implemented - even with the many constraints research staff work through daily - to improve their experience and your recruitment funnel.
The avoidable icebergs
Most of us see the tips of the icebergs that patients must navigate around in their search for a trial. We know, intuitively, that patients are busy and that they are not always medical experts. The problem is that we, as a field, do not investigate just how vast these icebergs are underneath the surface. Failure to fully understand the scope of the problems will only lead to a world where patient-centricity is a tossed-aside buzzword.
Here is what we've discovered about the icebergs after working directly with thousands of patients.
Learning about the clinical trial
When first learning about a trial, patients consistently want to know four main things.
- Can this trial potentially help me?
- Does it look like I’m eligible?
- Is it feasible (financially and logistically) for me to participate?
- What is the next step to see if I can join the study?
Today, most patients have at most two of those questions answered by the trial listing they find, often buried in very complicated language, terms, and abbreviations that are foreign to them. Looking at a typical listing, with its complex language and inscrutable formatting, the patient has to make a decision: Is it worth even more of their time to find out whether this trial is relevant to them?
For some patients, the answer is, Yes. For many others, the answer is, I'd love to, but I don't have the time or energy or resources or sense of empowerment.
Looking at a typical listing, the patient has to make a decision: Is it worth even more of their time to find out whether this trial is relevant to them?
Inquiring about the clinical trial
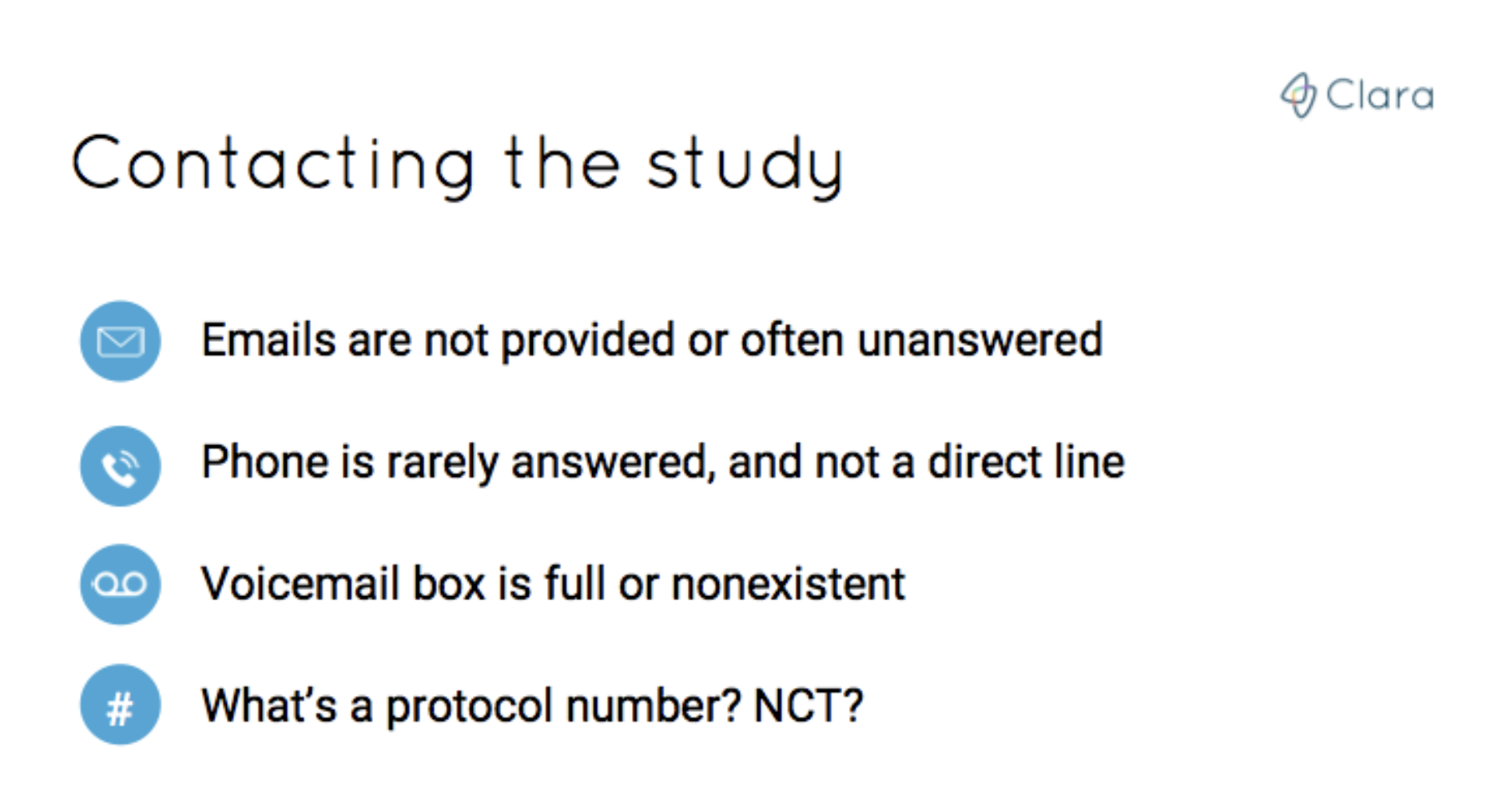
If the patient does decide that it’s worth their time, they’ll usually look for contact information, which in most cases is a phone number or email listed on the trial listing.
But email inquiries will go unanswered for weeks. The phone number listed will either be incorrect or outdated (or no one will pick up). Or the number leads to the front desk attendant of the research site or hospital or pharmaceutical company's headquarters...and they have no idea what the patient is trying to inquire about (and why would they?).
A motivated patient will spend this time in ambiguity to run some Google cross references. They will copy and paste the words and acronyms they didn't understand to find out whether there is another resource they could be looking to. They'll post their questions on patient communities and social media.
But most of the time, even the most motivated patient will feel intimidated by the language and the work required to even reach someone who can answer their questions. Eventually, many of them fall out of the recruitment funnels of the trials that they were so excited about at the beginning of their search.
Imagine attempting to book a hotel room, only you must book through the phone, and then there’s only a 15% chance that anyone you speak to (if you do manage to speak to anyone at all) has even a slight idea as to what you’re trying to accomplish. How many attempts would you make before deciding to try booking a different hotel or doing a staycation instead?
If the patient is lucky or persistent enough to speak with a coordinator, they’re often asked for a protocol number so the researcher knows what study they’re referencing. That should be fine, but the listing page the patient found didn’t mention a protocol number. Now they’re either at a dead end, and must hang up to try to find this number and call back. Or they must wait to get a callback from someone else who can help.
Spoiler alert (a predictable one): The patient doesn’t usually get a call back.
We know this firsthand.
We made these phone calls ourselves on behalf of patients. We sent the emails. We even built internal tools to automate outreach to clinical trial sites...and even our team got overwhelmed in this maddening maze. If we - with our software designed specifically for this task and tracking spreadsheets and generally solid understanding of the language and nuances of clinical trials - got lost here, what chance does an average patient have?
Imagine attempting to book a hotel room, only you must book through the phone with only a 15% chance that anyone you speak to has even a slight idea as to what you’re trying to accomplish.
Needless to say, the clinical trial team has clearly lost some interested candidates by this point, and this is only the first part of the funnel.
Screening
Still, the persistent patient does eventually reach someone who can administer a pre-screener survey, and sends over their medical record to them. If the patient knows how to access their medical record like the back of their hand, this step is a breeze.
Unfortunately, that’s often not the case. A study from the HHS found that only 52 percent of patients in 2017 were offered online access to their medical record by a health provider. When a patient gets asked to find or send over their medical records, they aren't exactly handed a detailed map on how to do that. This leads to even more delay, more phone tag, and more frustration-driven drop-off.
Still, as before, some patients make it to the next step. The patients who were able to gather all of their information and complete the pre-screener will need to wait to hear the results, and then coordinate another call in order to schedule the next step, commonly a physical screener at the trial site. And what tends to happen during this process? More drop-off.
Only 52 percent of patients in 2017 were offered online access to their medical record.
By now, the patient who has a scheduled screening appointment has spent hours on gathering documents, calling and email, and speaking to a string of staff members. Imagine how frustrating it would be for this patient to show up for their screening and consent appointment, only to find that the medical staff at the center aren’t even familiar with the trial that the patient has come to screen for.
It sounds comically absurd, but this is something that just happened last month with a patient we’ve been helping. The patient was sent back home and told to try contacting the coordinator once again.
Which they tried unsuccessfully to do.
For over two weeks.
Unfair allocation of responsibility
Patients carry an unfair portion of the responsibility when attempting to enroll in a trial, as they are forced to get through all of these points of frustration while also managing their medical condition, work, family, and the many other considerations of their everyday lives.
These are the hurdles that we’ve helped patient after patient navigate. Unfortunately, these hurdles aren’t exceptions to the rule - they are the common thread that tie together most patient experiences when interacting with clinical trials. Over the years, we’ve honed our own approach to clinical trials, as it pertains to both patient experience and to trial recruitment design.
We’re excited to share a few of our best practices as actionable steps that you can take as a clinical trial sponsor, site, or individual team member.
Patient-centric solutions
1. Clinical trial information resources
Let's go back to the beginning.
There is the patient, in front of their computer or tablet or on their smartphone, and they are squinting from the effort of scrutinizing a trial listing. There is a good chance that this patient will give up from the frustration.
A future holiday traveler feels excitement at the potential of new discoveries in new places when they visit Airbnb to book a home or an experience; we need to ensure that the beginning of the enrollment process similarly conveys to any patient the potential of new treatment and addresses their most common worries immediately and in clear language.
The good news is that no one has to be as well-staffed as Airbnb to improve this top-of-funnel experience.
Simply ensuring that an easy-to-read and easily accessible resource that answers four key questions is made available to the patient wherever your team reaches them can fix a bulk of these problems.
1. Can this trial potentially help them?
This can be answered with past data or why the research team thinks the treatment may work.
2. Are they likely eligible?
This can be articulated with a clear breakdown of the basic eligibility criteria, or better yet, by using a HIPAA-compliant pre-screener embedded directly in the listing.
3. Is it financially and logistically feasible to take part in the trial?
To answer this the patient needs to understand if the cost of treatment is covered, if travel reimbursement is available and what that can cover, and how frequent and long the visits usually are. This last one’s important because it impacts if they will have to miss work, or hire a nanny for the kids, and that could make the study impossible for them.
4. Most importantly, what is the next step to see if they qualify?
The next step should be clear, easy to take, and immediate.
These questions should be answered everywhere you are engaging patients. If you’re working to reach patients online, these details should be delivered in the form of a landing page or listing about your clinical trial. When you’re reaching patients in the waiting room, adapt the materials to a pamphlet or flyer. If you're going directly into the community and speaking to patients one-on-one, ensure that you are addressing each of these four questions, whether they are explicitly asked or not.
Quick thoughts on clinical trial landing pages
Taking the extra time in creating patient-centric pages may add time to a team's startup phase. But, as patients come in better-informed and more ready to enroll, and as the research team's time is focused less on returning emails and administering prescreens by phone, the upfront time investment will yield far more productivity down the road.
For example, each of Gilead’s FINCH studies for rheumatoid arthritis have dedicated websites and are a great example of providing understandable information to patients.
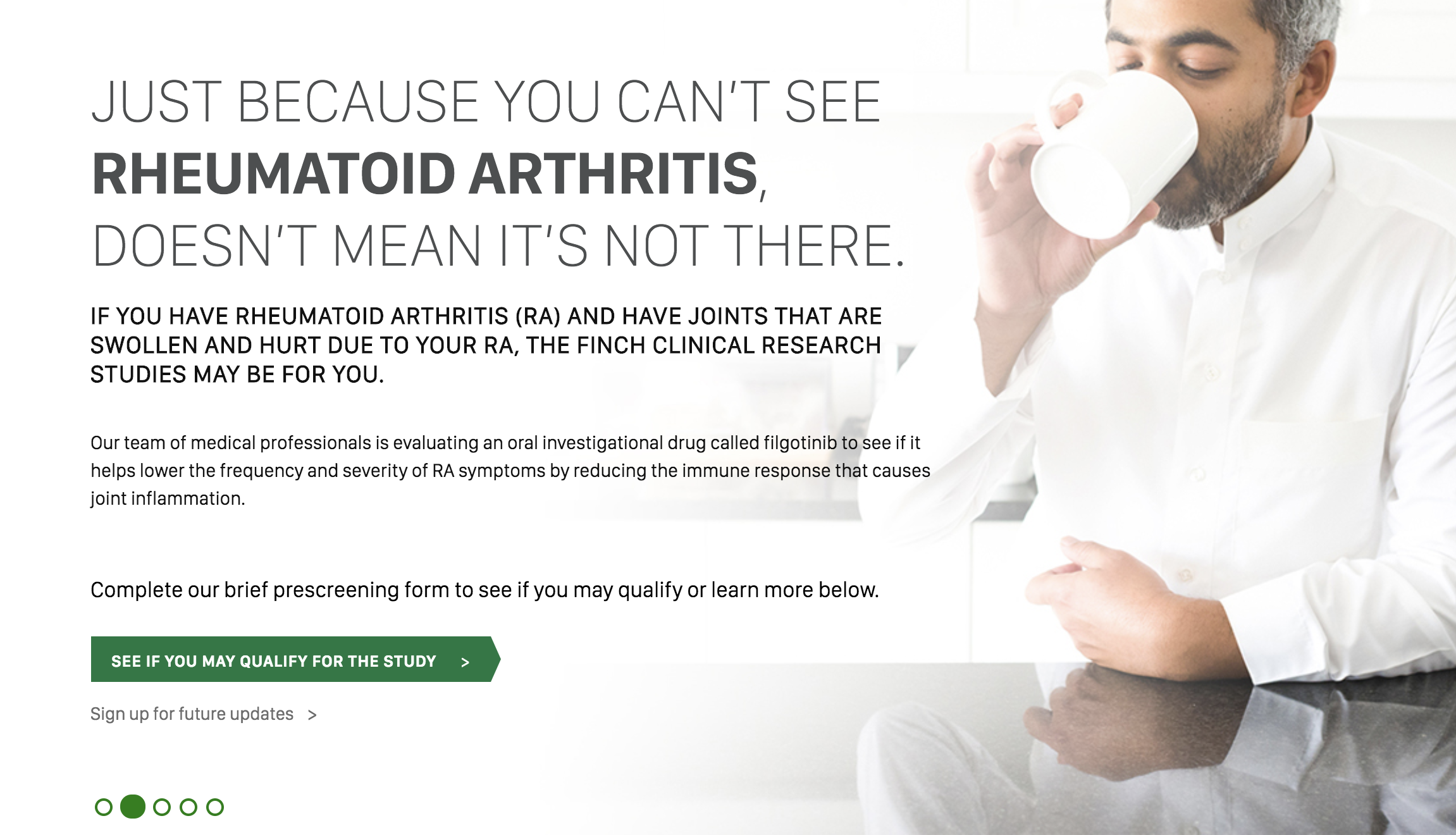
Their clinicaltrials.gov listing links to this optimized and friendly landing page. And the language here is far easier to read and explains in plain English what patients are most interested in knowing. They even have a clear call to action button (“See if you may qualify for this study”) for interested patients who want to apply, which leads patients to a built-in pre-screener.
At Clara, we’ve seen great improvement in listing conversion rates when a pre-screener survey is embedded in the trial listing itself.
By embedding such a survey, your landing page does the pre-screening work for you and your team, and converts pre-qualified visitors into prospective enrollees in mere seconds. Pre-screeners also provide the patient much-need flexibility by providing a longer period of time in which they are free to look up their medical information and provide answers, without taking time from your research team.
We use seven tactics on any landing page we create for the trials we work with. You can read about them here.
2. Following up with candidates
When modern consumers are met with unexpected delays, they have no problem looking elsewhere. Every consumer company in the world from Domino's to Facebook understands this. And when working with patients the need for responsiveness is all the more acute as they labor to balance the many responsibilities of work, family, and the management of their own medical conditions.
We built tools here at Clara that allow us to measure our response times in seconds; our target response time is actually 20 seconds. While that target may well be impossible for those working manually, we still advise any clinical trial to respond to emails and phone calls within 24 hours. Patients simply will not wait around; if they found your trial, chances are that they have found a number of others.
Be responsive. Here are some steps that any team can use to decrease response times.
Templatizing responses
Templated responses can greatly reduce the time it takes to get back to a patient. Here’s an example of a template:
“Hi Evan - thank you for reaching out! Here are some details for the study you asked about. I also attached the questionnaires that need to be completed so we can see if you qualify.
CLAR-39182 STUDY DETAILS
There is a visit to the study site every 2 weeks, with 10 visits in total.
Each visit lasts from 3:30pm-5pm.
You'll receive a stipend for participating in the study, which is $100 per visit.
You may stay on all of your current medications during the trial.
Please feel free to contact by phone or email with any questions.
Thanks, Clara"
There's no need to reinvent the wheel here. A simple response that outlines some basic information about the study can go a long way.
Having a templated response ready to go will help you minimize the workload of responding to each new inquiry and ensure that each patient is given a quick, informative response. Templates can also enable your team to set up automated responses to ensure that any inbound email gets a templated email response that confirms receipt and ensures the recipient that someone will be in contact within 24 business hours.
Here are tutorials for how to set up autoresponses in Outlook and in Gmail.
Scheduling appointments and calls
Once a patient has been pre-qualified, teams should move as quickly as possible to schedule a phone call or an onsite visit.
The best time for this is either immediately after they have successfully completed a pre-screening survey, or in the immediate couple of days following. Waiting longer could lead to the patient forgetting about the details of the study, moving on to a different treatment option, or deciding they don’t want to proceed with applying.
When booking time with a patient it’s beneficial to send them a digital calendar invite. If the patient has a smartphone, an accepted calendar invite for a scheduled phone call or visit will trigger automatic notifications on their phone or email to remind them in advance of the appointment, even if they don’t normally use their calendar app much.
We like to use a simple tool like calendly at Clara. These sorts of tools can offload the work from your team of manually scheduling appointments, and gives the patient greater flexibility in finding times that work best for them. Of course, if you have the bandwidth, a personalized email or phone call to remind them never hurts.
Setting up trial-specific phone lines and voicemails
For phone calls, direct patients to a line that is specific to that particular trial and your site.
This can be done using free services like Google Voice. Setting up different lines for different trials enables your team to know immediately which trial a patient is interested in when they call. It even allows the team to record custom voicemails specific to the trial the patient is calling about, and provides the option for patients to text in lieu of a call. Of course, checking the voicemail and responding to all new inquiries at least once a day ensures a great experience for any patient.
3. Helping gather electronic medical records
The level of experience varies from patient to patient when it comes to accessing electronic health records. In our experience, it's best to assume that the patient has little experience in navigating their online portals - being overly helpful at this stage doesn't hurt, but being presumptive about a patient's comfort with these tools can definitely be detrimental.
It's the case, though, that many teams are too busy to be very hands-on with this process. We've met a number of teams who built services that will aggregate and organize all of the medical records from multiple hospitals on a patient’s behalf. One we can recommend from experience is Picnic Health -- their services can help augment your team's ability to help patients through what should be a simple - but sadly can be anything but - step.
4. Keeping all the information in one place
By the time a patient comes in for their visit and is ready to enroll into the trial, it is almost always the case that the research team has done a fantastic job answering the patient’s questions and clearly laying out the next steps. However, participants can forget the next steps, or might realize they had other questions they wanted answered.
Being able to have a “home base” of resources, answers, and contact information can help them troubleshoot their concerns faster and increase their likelihood to continue through the entire trial. Keeping these resources available as PDF files and as printed, physical copies can do wonders in helping keep interested patients on top of the many steps that make up the enrollment process.
5. Add “moments of delight”
When selling to consumers, there is an idea referred to as “moments of delight.” This is a moment of unexpected surprise that brings a smile to the customer's face. Think about Google’s homepage and how it changes to celebrate events like Martin Luther King, Jr. Day. Or how novel it was to hear Siri crack a joke for the first time (admittedly, her jokes aren’t quite funny enough to paper over her limited functionality, but that’s for another essay on another day).

By offering these small moments of appreciation to your applicants, enrollees, and their caregivers, a real relationship can be developed with them, which leads to increased engagement and retention through their application process and eventual trial participation.
The ways we’ve gone about this at Clara are through offering highly personalized touches, such as hand-written cards signed by the entire team or even small care packages containing items that make hospital visits cozier, such as warm socks and blankets.

By looking for various ways in which we can delight our community, we’ve been able to build an authentic connection with our members, which makes those inevitable moments of frustration (due to slow responses from trial sites, or a disappointing failed pre-screen) that much easier to navigate together.
6. Tracking metrics to optimize your process
It is common practice for teams to run a retrospective on the data collected from a recently-enrolled study to answer questions like “How many referred patients ended up enrolling” or “Why did most of the unenrolled choose not to proceed?”
However, it is equally important to run continuous analysis on a study’s recruitment funnel, even while recruitment efforts are ongoing.
In this case, another parallel to the world of consumer technology can be drawn: Companies such as Twitter and Facebook track detailed metrics such as average visit length, daily active users, and the ratio of daily active users over monthly actives (among a thousand other figures).
We look to 25 daily metrics at Clara to understand what is happening within the recruitment and how the funnel can be optimized, from visit-to-completed screener conversion rates to response times across sites. You can read and watch a detailed breakdown about our funnel analysis framework here.
It can be a challenge to obtain similar data from a clinicaltrials.gov listing, or from a third-party landing page created for you by a vendor. While the former is likely always going to be a bit of a black box, your study team can maximize its chances at recruitment success by choosing to work with vendors who not only can create landing pages but can also provide detailed performance data to your team on a real-time basis (and, yes, we do provide daily reports to every trial team we work with that details the measures that they are most interested in).
Monitoring metrics in this way makes for a much more agile recruitment effort, and helps increase the impact of all recruitment initiatives.
Implementation
It may seem like these steps require a lot of setup time, but the gains in team productivity and funnel conversion rate improvements vastly outweigh the setup costs. The end result of adopting this approach towards recruitment is an incredible experience for any patients considering your clinical trial and a much higher conversion rate from interest to enrolled, directly boosting your ability to recruit rapidly. By maximizing the impact of each stage of your recruitment funnel, you will bring in more qualified patients, faster and cheaper than your team previously could.
If you are already in the middle of a recruitment effort, it may not be feasible to run new language by your IRB, or have a new landing page built, or what have you. But some of these steps - automating responses to ensure a patient knows they were heard, providing comprehensive details on the questions patients ask most frequently, etc. - are feasible for any team, of any size, in any phase of their trial process. We challenge you to implement at least some of these principles into your recruitment efforts: The outcome will absolutely be worth the effort.
